-
Die Universität
- Herzlich willkommen
- Das sind wir
- Medien & PR
-
Studium
- Allgemein
- Studienangebot
- Campusleben
-
Forschung
- Profil
- Infrastruktur
- Kooperationen
- Services
-
Karriere
- Arbeitgeberin Med Uni Graz
- Potenziale
- Arbeitsumfeld
- Offene Stellen
-
Diagnostik
- Patient*innen
- Zuweiser*innen
-
Gesundheitsthemen
- Gesundheitsinfrastruktur
Case of the Month
April 2023
Small bowel resection from a 38-year-old male.
Diagnosis
Misplaced glands / enteritis cystica profunda in Peutz-Jeghers syndrome.
Comment
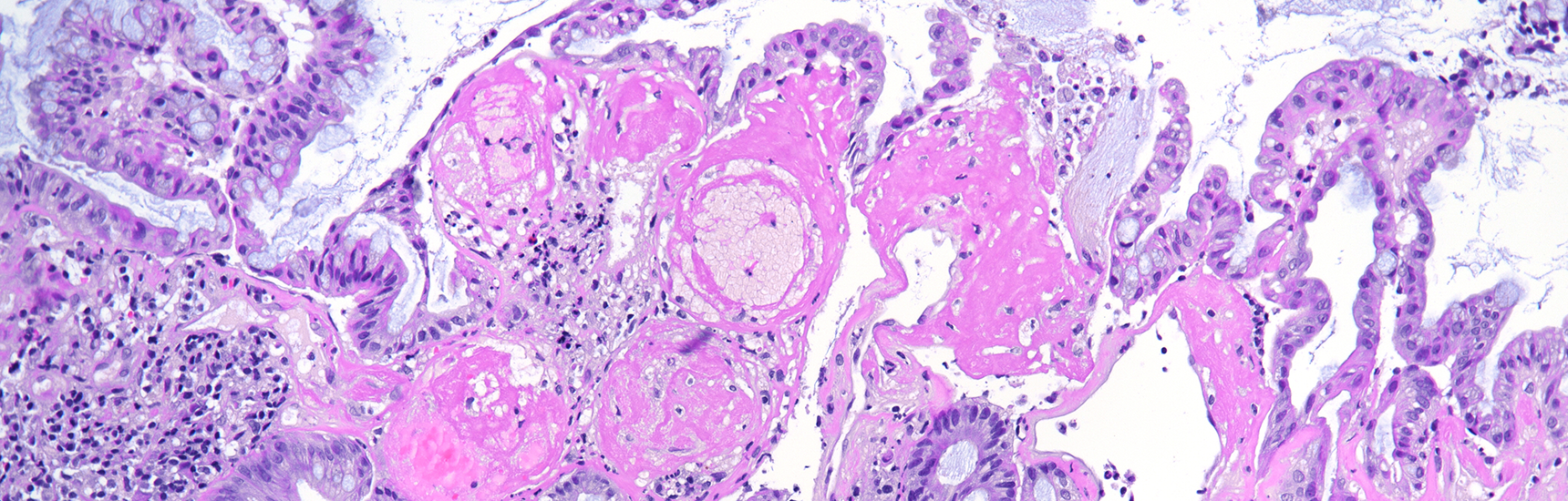
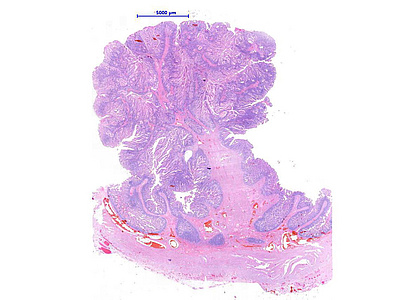
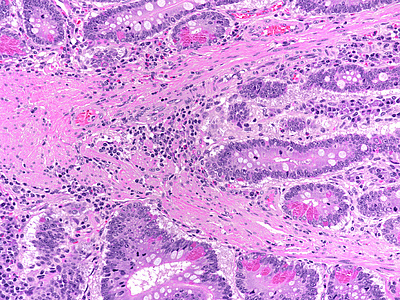
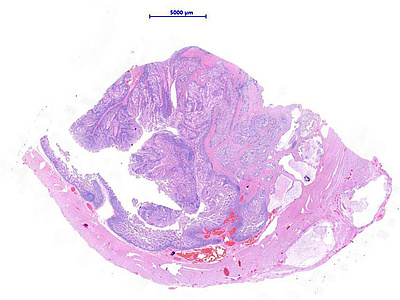
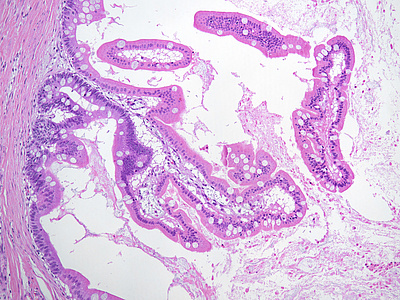
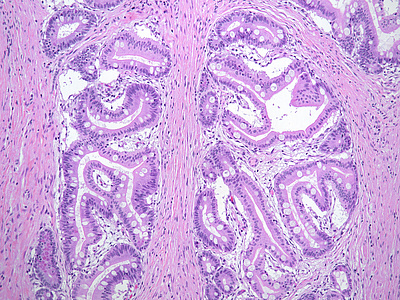
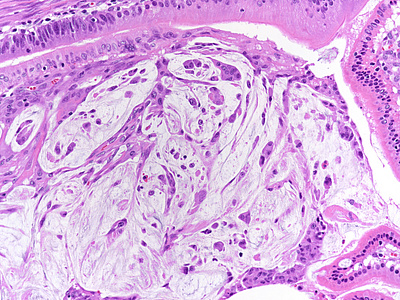
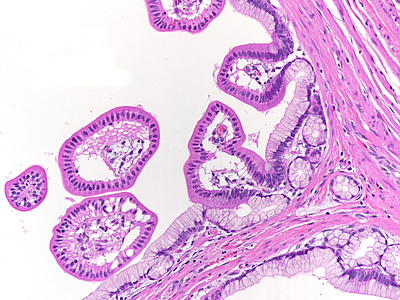
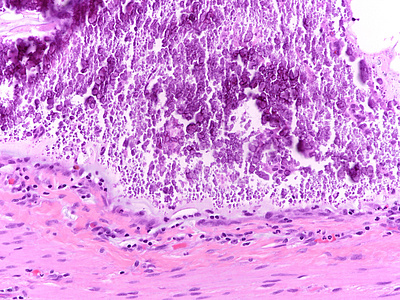
A 38-year-old male with known Peutz-Jeghers syndrome underwent small bowel resection. We observed a pedunculated polyp, which unveils a complex arborizing architecture with prominent branching smooth muscle bundles, derived from the muscularis mucosae (PANELS A-B). On high power, the villi are lined by native ileal epithelium without atypia. Beneath the polyp, in other step sections throughout the muscularis propria layer, we found misplaced glands, some of which in the form of mucin-filled cystic spaces, partially lined by villous structures, composed by the same epithelium as the polyp that were surrounded by lamina propria and lacking stromal desmoplasia (PANEL C-E). Detached, degenerated epithelial elements, which should not be mistaken for dysplasia / invasive mucinous carcinoma, were floating within the mucin (PANEL F). Areas of pyloric gland metaplasia (PANEL G) and calcification (PANEL H) were also found. Final diagnosis was Peutz-Jeghers polyp with misplaced glands / pseudoinvasion.
Peutz-Jeghers polyps are hamartomatous polyps, which may occur in syndromic context or sporadically, throughout the entire gastrointestinal tract, especially within the small bowel (65-90%). About 10% of small intestine Peutz-Jeghers polyps have foci of misplaced epithelium with herniation throughout the submucosa and muscularis propria, caused by prolapse and peristaltic kneading, producing a transmural enteritis cystica profunda configuration. This pseudo-invasive pattern is a well-recognized phenomenon, encountered more frequently in polyps larger than 3 cm in diameter, which implies a dangerous pitfall, since these polyps may be mistaken for malignancy. However, there are features that aid the discrimination between misplaced epithelium and malignancy. The following features favors a benign nature of the lesion: (i) lack of a true infiltrative growth pattern; (ii) presence of enteritis cystica profunda, with deep mucinous cysts; (iii) absence of atypical epithelium in the deep glands; (iv) presence of lamina propria surrounding the displaced glands; and (v) absence of stromal desmoplasia. Dysplasia is rare in Peutz-Jeghers polyps, and malignancy has only anecdotally been reported.
For further reading
- Shaco-Levy R, Jasperson KW, Martin K, et al. Morphologic characterization of hamartomatous gastrointestinal polyps in Cowden syndrome, Peutz-Jeghers syndrome, and juvenile polyposis syndrome. Hum Pathol. 2016; 49: 39-48.
- Jansen M, de Leng WWJ, Baas AF, et al Mucosal prolapse in the pathogenesis of Peutz-Jeghers polyposis Gut. 2006; 55:1-5.
- Petersen VC, Sheehan AL, Bryan RL, Armstrong CP, Shepherd NA. Misplacement of dysplastic epithelium in Peutz-Jeghers Polyps: the ultimate diagnostic pitfall? Am J Surg Pathol. 2000; 24(1):34-9.
- Bolwell JS, James PD. Peutz-Jeghers syndrome with pseudoinvasion of hamartomatous polyps and multiples epithelial neoplasm. Histopathology. 1979; 3(1):39-50.
Presented by
Dr. Rafael Moiteiro da Cruz, Lisbon, Portugal and Dr. Cord Langner, Graz, Austria.