-
Die Universität
- Herzlich willkommen
- Das sind wir
- Medien & PR
-
Studium
- Allgemein
- Studienangebot
- Campusleben
-
Forschung
- Profil
- Infrastruktur
- Kooperationen
- Services
-
Karriere
- Arbeitgeberin Med Uni Graz
- Potenziale
- Arbeitsumfeld
- Offene Stellen
-
Diagnostik
- Patient*innen
- Zuweiser*innen
-
Gesundheitsthemen
- Gesundheitsinfrastruktur
Case of the Month
August 2022
Biopsy from a gastric ulcer in a 41-year-old female.
Diagnosis
Drug-induced injury by arterial chemoembolization (TACE) with fotemustine.
Comment
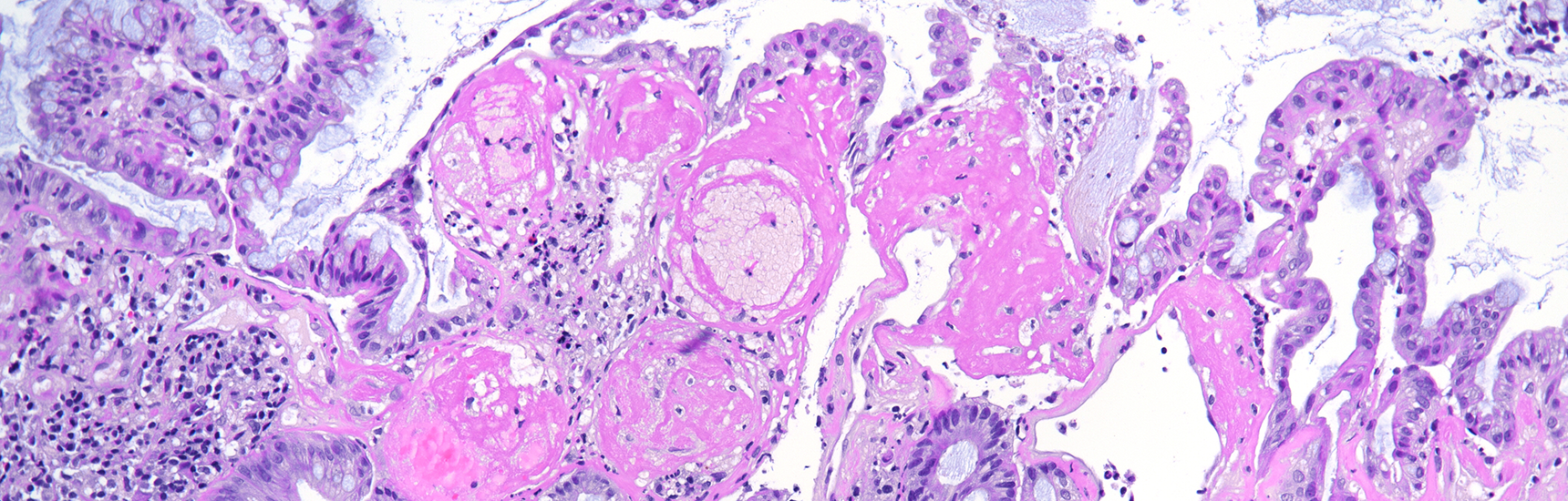
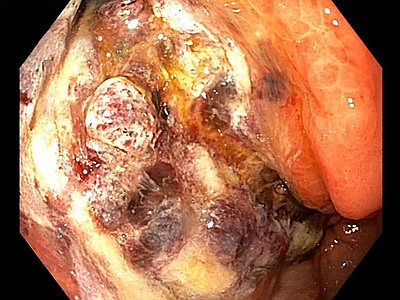
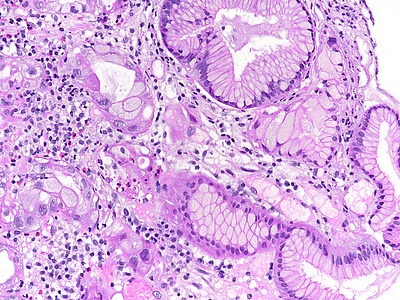
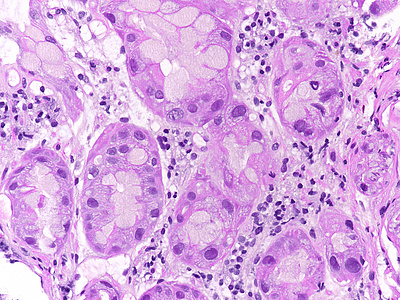
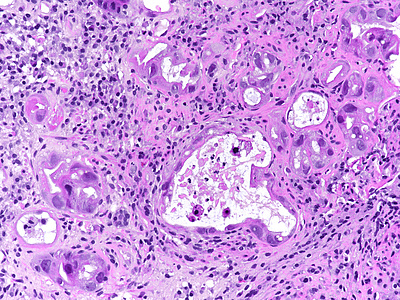
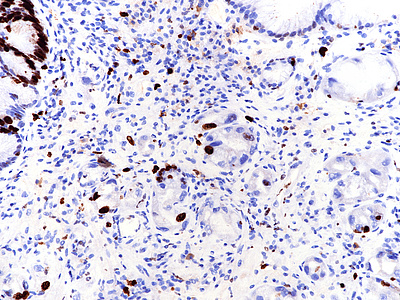
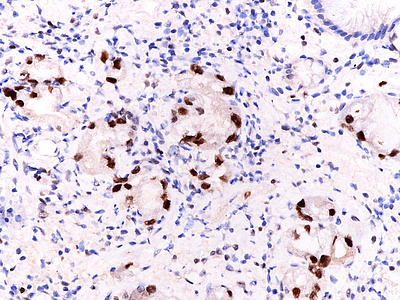
A 41-year-old female with ocular malignant melanoma, metastatic to both lobes of the liver, presented with nausea, vomiting and epigastric pain. Upon endoscopy, a large ulcerated lesion, extending from the corpus to the duodenal bulb, was detected (Panel A). Upon histology, ballooning cells with mild to moderate nuclear atypia were observed within the surface and foveolar epithelium (Panel B-C). Marked nuclear pleomorphism, hyperchromasia and loss of polarity, along with increased cytoplasmic eosinophilia were present within the deep gastric glands (Panel D). Mitotic figures were not seen, and the Ki-67 labelling index was low (Panel E). p53 overexpression was noted in the atypical cells, however with heterogeneous staining, thereby indicating an activated wild-type pattern (Panel F).
Metastatis to the liver may be managed by local ablative therapies such as transarterial chemoembolization (TACE). Fotemustine is a nitrosourea alkylating agent that is used to treat metastatic melanoma. Gastroduodenal ulcers are a rare complication of TACE, which may be explained by the shared origin of hepatic and gastroduodenal arteries.
The presented case demonstrates severe atypia of the gastric epithelium, which exceeds what is typically seen in ischaemic injury and may lead to the erroneous diagnosis of dysplasia and/or malignancy. Drug toxicity explains these findings. Specifically, fotemustine causes interstrand crosslinking of DNA, which prevents DNA replication, and ultimately leads to apoptosis in a p53 dependent manner. Interestingly, Ki-67 labeling was low in our case. This may be attributable to the fact that the highest levels of nuclear Ki-67 staining are reached during the M phase of the cell cycle, which the epithelial cells failed to enter due to the drug effect (Varelas et al. 2022).
It is of note that intense staining of p53 (overexpression within a wild-type pattern) has been reported from ischemic bowel disease or as consequence of other anti-tumour treatment modalities, such as selective internal radiation therapy (SIRT) using Yttrium microspheres. Pathologists need to be aware of this important pitfall.
For further reading
- Crowder CD, Grabowski C, Inampudi S, Sielaff T, Sherman CA, Batts KP. Selective internal radiation therapy-induced extrahepatic injury: an emerging cause of iatrogenic organ damage. Am J Surg Pathol. 2009 Jul;33(7):963-75. doi: 10.1097/PAS.0b013e31817ed787.
- Schuster R, Lindner M, Wacker F, Krössin M, Bechrakis N, Foerster MH, Thiel E, Keilholz U, Schmittel A. Transarterial chemoembolization of liver metastases from uveal melanoma after failure of systemic therapy: toxicity and outcome. Melanoma Res 2010; 20: 191-196.
- Agarwala SS, Eggermont AMM, O'Day S, Zager JS. Metastatic melanoma to the liver: a contemporary and comprehensive review of surgical, systemic, and regional therapeutic options. Cancer 2014; 120: 781-789.
- Abraham SC, Taggart MW, Loftus Jr EV, Wu TT. Dysplasia-like epithelial atypia in ischemic bowel disease. Hum Pathol 2014; 45: 1348-1357.
- Chintalapati SP, Patel A, Conjeevaram H. Gastric and duodenal ischaemia after transarterial chemoembolisation for hepatocellular carcinoma: an unexpected but significant complication. BMJ Case Rep 2018 Feb 21;2018:bcr2017223339
- Varelas AI, Kővári B, Bruckner E, Lauwers GY, Langner C. Metachronous double-hit by arterial chemoembolization (TACE) with fotemustine inducing dysplasia-like atypia in the gallbladder and stomach - a diagnostic pitfall. Histopathology. 2022 Mar 22. doi: 10.1111/his.14653. Online ahead of print.
Presented by
Dr. Ana Varelas, Porto, Portugal, and Dr. Cord Langner, Graz, Austria.