-
Die Universität
- Herzlich willkommen
- Das sind wir
- Medien & PR
-
Studium
- Allgemein
- Studienangebot
- Campusleben
-
Forschung
- Profil
- Infrastruktur
- Kooperationen
- Services
-
Karriere
- Arbeitgeberin Med Uni Graz
- Potenziale
- Arbeitsumfeld
- Offene Stellen
-
Diagnostik
- Patient*innen
- Zuweiser*innen
-
Gesundheitsthemen
- Gesundheitsinfrastruktur
Case of the Month
January 2022
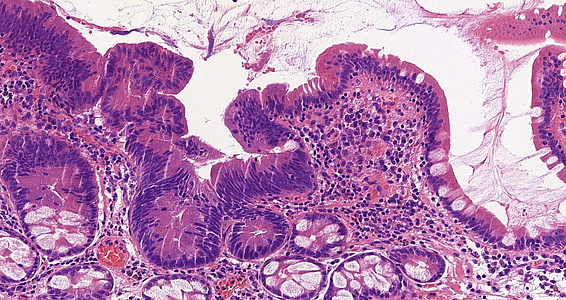
60-year-old female, biopsy referred to be from the Vater papilla.
Diagnosis
Tubulovillous adenoma with low-grade dysplasia.
Comment
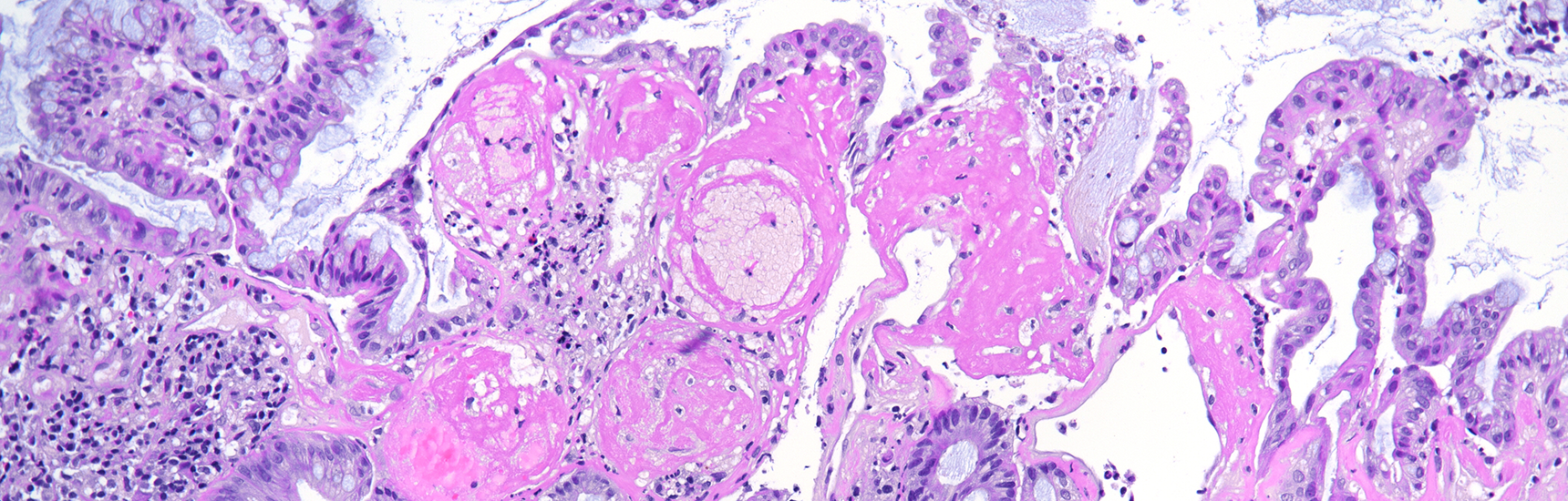
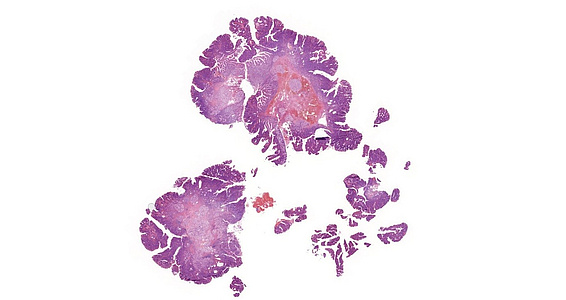
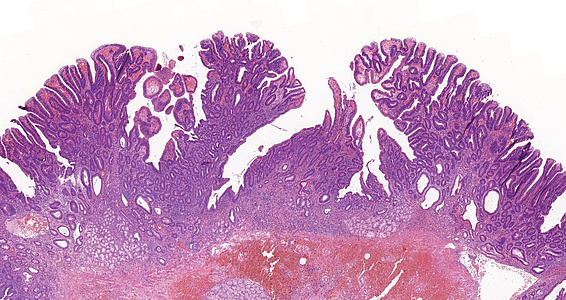
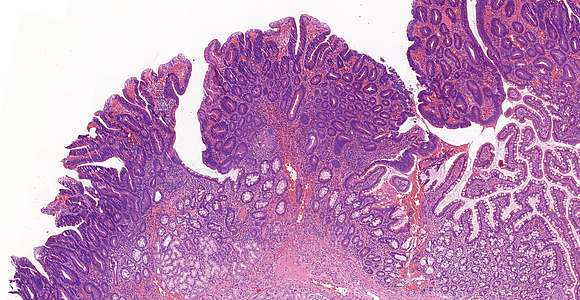
A 60-year-old female patient underwent multiple gastroscopies during the last 5 years because of recurring jaundice. Biopsy samples of the Vater papilla were taken each time, showing tubular or tubulovillous adenomatous growth. In 2021, the lesion was resected in toto with sphincteroplasty. Microscopic examination of this sample revealed tubular and tubulovillous structures, showing signs of low-grade dysplasia (revised Vienna classification category 3) in continuation with normal mucosa [Panels A-D]. Brunner glands were present in the submucosa. Even though the resection margin was free of dysplasia and invasive malignancy not detected, careful follow-up was recommended due to the patient’s history and the recurring nature of the lesion.
Neoplastic lesions of the papilla of Vater are generally rare (0.1-0.2% of all gastrointestinal tumours). Neoplastic lesions include adenomas and adenocarcinomas, but due to the anatomic location, pancreatic adenocarcinomas and cholangiocarcinomas can also be found. Tubulovillous adenomas are premalignant lesions. According to Onkendi et al., 44% of benign Vater papilla lesions proved to be tubular adenomas, while 45% were tubulovillous adenomas, and 11% showed pure villous morphology. These adenomas rarely cause symptoms, but with increasing size, they may cause jaundice, biliary colic, pancreatitis or upper gastrointestinal bleeding.
Adenomas of the papilla of Vater are mainly sporadic, although association with familial adenomatous polyposis (FAP) has been noted. Of note, diagnosis of duodenal, Vater papilla or (peri-)ampullary adenomas should always prompt thorough examination of the colon to identify possible synchronous neoplastic lesions.
Therapeutical options generally include local endoscopic procedures, such as ampullary resection, duodenotomy or duodenopancreatectomy, in particular when local excision is not possible technically or in cases with suspected malignancy. The presence of high-grade dysplasia, histological subtype, multiplicity, the localisation of the lesion and the increase in size of the adenoma has a significant correlation with the recurrence rate and always raises suspicion for invasion. Hence, resection margins always have to be examined thoroughly.
For further reading
- Fernandes DA, Boteon YL, Boteon APCS, et al. Tubulovillous adenoma of the duodenal papilla: radiological-endoscopic and anatomopathological correlation in the surgical proposal. Rev Assoc Med Bras. 2020; 66: 1190-1195.
- Bellizzi AM, Kahaleh M, Stelow EB. The assessment of specimens procured by endoscopic ampullectomy. Am J Clin Pathol. 2009; 132: 506–513.
- Heidecke CD; Rosenberg R; Bauer M, et al. Impact of grade of dysplasia in villous adenomas of vater’s papilla. World J Surg. 2002; 26: 709–714.
- Onkendi EO, Naik ND, Rosedahl JK, et al. Adenomas of the ampulla of Vater: a comparison of outcomes of operative and endoscopic resections. J Gastroint Surg. 2014; 18: 1588–1596.
- Nikolaidis P, Hammond NA, Day K, et al. Imaging features of benign and malignant ampullary and periampullary lesions. Radiographics. 2014; 34: 624-641.
- Alexiou K, Ioannidis A, Drikos I, et al. Adenoma of the ampulla of Vater: a case report. J Med Case Reports. 2018; 8: 228.
Presented by
Dr. Szintia Almási, Szeged, Hungary, Dr. Anita Sejben, Szeged, Hungary.