-
Die Universität
- Herzlich willkommen
- Das sind wir
- Medien & PR
-
Studium
- Allgemein
- Studienangebot
- Campusleben
-
Forschung
- Profil
- Infrastruktur
- Kooperationen
- Services
-
Karriere
- Arbeitgeberin Med Uni Graz
- Potenziale
- Arbeitsumfeld
- Offene Stellen
-
Diagnostik
- Patient*innen
- Zuweiser*innen
-
Gesundheitsthemen
- Gesundheitsinfrastruktur
Case of the Month
March 2022
A 51 year-old woman with an expansive appendiceal mass, clinically suspected to be a neuroendocrine tumour.
Diagnosis
Appendiceal schwannoma.
Comment
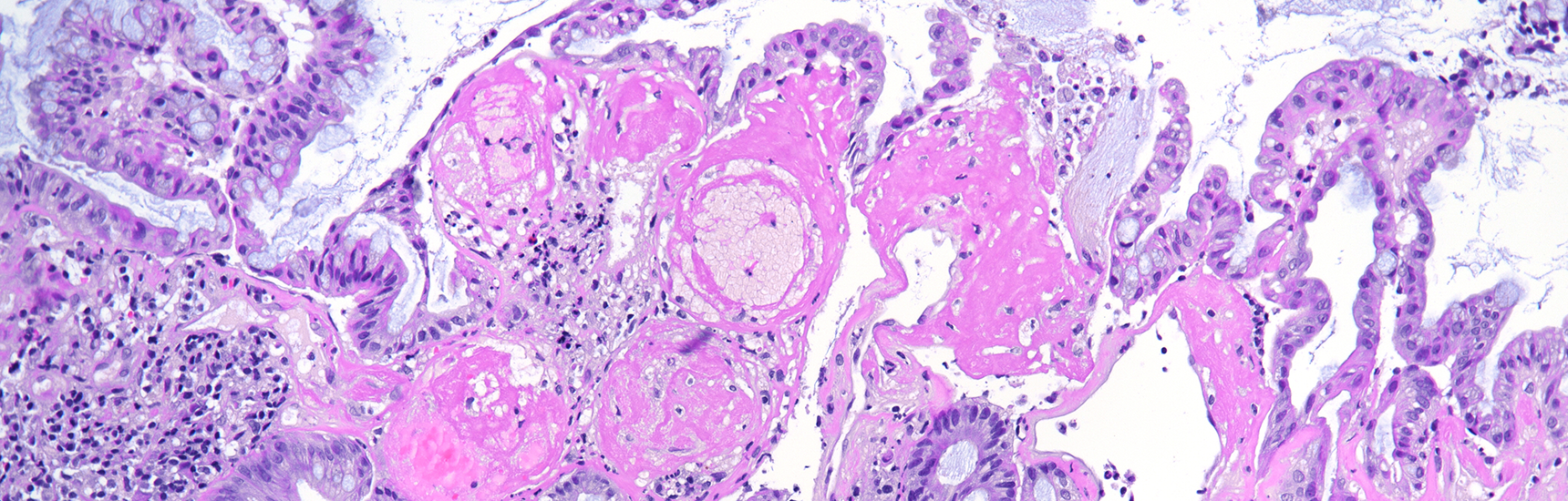
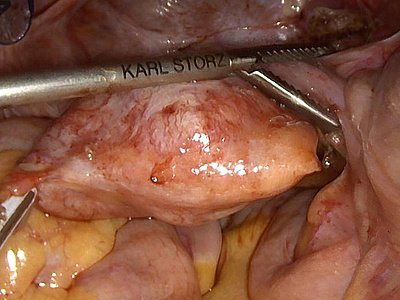
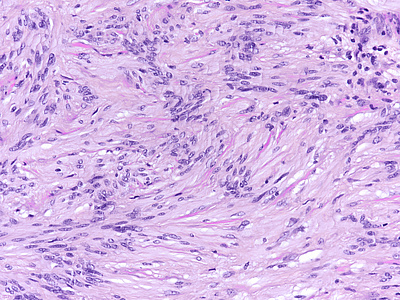
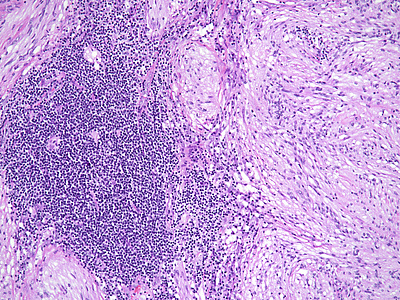
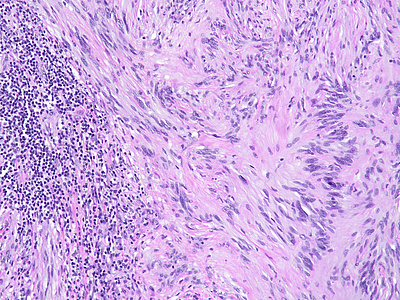
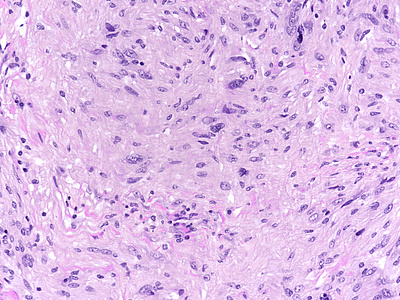
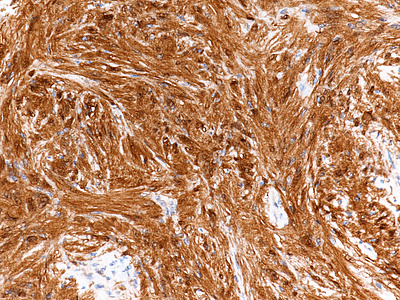
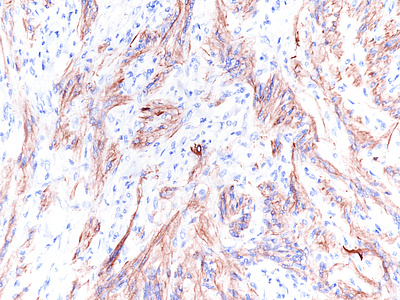
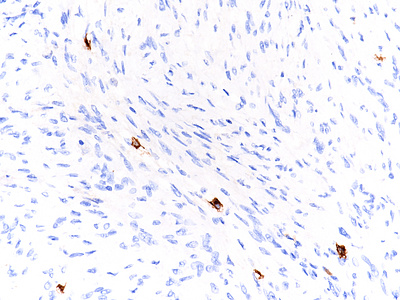
During laparoscopic surgery, the tumour proved to be confined to the appendix, with no other intra-abdominal findings (Panel A). The resection specimen disclosed a well circumscribed solid tumour, 4.2 cm in maximum diameter, with a homogeneously yellowish-white cut surface (Panels B and C). Histologically, we observed a loose to densely cellular, spindled-cell neoplasia, arranged in fascicular and sweeping patterns (Panel D). Lymphoid aggregates, sometimes forming lymphoid follicles with germinal centres, were found distributed at the periphery and also throughout the tumour (Panels E and F). The neoplastic cells had sparse cytoplasm and elongated, bland nuclei with inconspicuous nucleoli; focal and moderate atypia was noted (Panel G). Mitotic activity was <5mitoses/10HPF. Haemorrhage or necrosis were not observed. Upon immunohistochemistry, there was diffuse and strong positivity for S100 protein (Panel H) and moderate positivity for GFAP (Panel I). CD117 marked intralesional mast cells, whereas the tumour cells were negative (Panel J). Desmin and smooth muscle actin were negative (not shown).
Schwannomas can occur anywhere in the gastrointestinal tract, mostly in the stomach. It is of note that gastrointestinal schwannomas lack some of the most typical features of its soft tissue counterparts, including encapsulation, well-formed Verocay bodies and hyalinized vessels. Furthermore, schwannoma is a very rare diagnosis in the appendix; currently, less than 20 cases of appendiceal schwannomas were reported in the literature.
Clinically, patients may present as acute/subacute appendicitis or may be asymptomatic, the appendiceal mass lesion being an incidental finding on image analysis performed for other reasons. The differential diagnosis of spindled neoplasm in the appendix includes gastrointestinal stromal tumour (GIST), leiomyoma, other benign peripheral nerve sheath tumors (neurofibroma, perineurioma, hybrid benign peripheral nerve sheath tumours) and malignant peripheral nerve sheath tumour (MPNST).
The characteristic morphology directs to the correct diagnosis: a well-circumscribed lesion, with a marbled appearance due to densely cellular areas alternating with densely cellular areas; and neoplastic spindled cells, sometimes with focal, degenerative atypia. Lymphoid cuffs, usually present in soft tissue schwannomas, have an unclear aetiology; in the appendix, its presence probably is due to remnants of local MALT-tissue. Long fascicular pattern, an epithelioid appearance, tumoral necrosis and increased mitotic activity must raise concern for malignant transformation to MPNST.
Confirmation by immunostaining is required given the mimicry of many mesenchymal tumours and the rarity of appendiceal schwannomas. A characteristic finding is the strong and diffuse positivity for S100 protein. Variable staining for GFAP and CD34 is present. Markers for GIST (CD117, DOG-1) are negative and positivity in Cajal cell hyperplasia or in scattered intralesional mastocytes is an important pitfall to consider. Also, muscle markers (desmin, smooth muscle actin) must be negative.
Appendiceal schwannomas have an excellent prognosis; appendectomy with clear resection margin is the curative treatment of choice.
For further reading
- Alkhattab M, Dhannoon A, Sehgal R, Gormley C, Sheehan M, Mclaughlin R. Schwannoma of the Appendix Orifice. Case Reports in Pathology. 2021; 2021: 1-4.
- Miettinen M, Sobin L. Gastrointestinal Stromal Tumors in the Appendix. The American Journal of Surgical Pathology. 2001; 25: 1433-1437.
- Misdraji J, Graeme-Cook F. Miscellaneous conditions of the appendix. Seminars in Diagnostic Pathology. 2004; 21: 151-163.
Presented by
Ana Isabel Varelas, Porto, Portugal, and Alexander Szyskowitz and Cord Langner, Graz, Austria.