-
Die Universität
- Herzlich willkommen
- Das sind wir
- Medien & PR
-
Studium
- Allgemein
- Studienangebot
- Campusleben
-
Forschung
- Profil
- Infrastruktur
- Kooperationen
- Services
-
Karriere
- Arbeitgeberin Med Uni Graz
- Potenziale
- Arbeitsumfeld
- Offene Stellen
-
Diagnostik
- Patient*innen
- Zuweiser*innen
-
Gesundheitsthemen
- Gesundheitsinfrastruktur
Case of the Month
August 2025
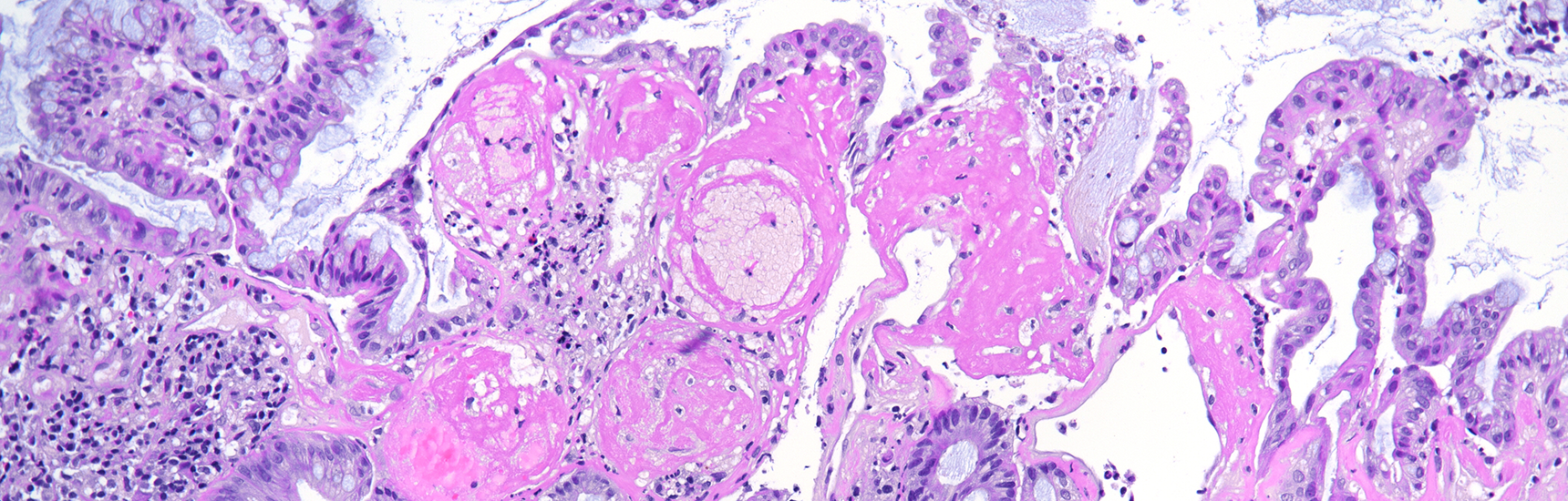
Biopsy from the ascending colon in an 87-year-old woman.
Diagnosis
Colorectal signet-ring cell carcinoma.
Comment
An 87-year-old female patient presented with iron deficiency anemia. Endoscopy showed in the ascending colon, a stenotic, centrally ulcerated lesion measuring 5cm in greatest dimension. Biopsies were performed, followed by right hemicolectomy.
Histology showed a diffusely infiltrative solid neoplasm, extensively involving the colonic wall, with ulceration of the mucosa and extension into the subserosa. The tumor was composed predominantly of poorly differentiated neoplastic cells, isolated or in small clusters, displaying prominent intracytoplasmic mucin vacuoles displacing eccentric, hyperchromatic nuclei to the periphery (Panels A-C), features diagnostic of signet-ring cell morphology. Focal areas showed extracellular mucin lakes, but no conventional gland-forming adenocarcinoma component was identified. Prominent lymphovascular invasion was evident. No lymph nodes with metastases were found.
Immunohistochemistry revealed diffuse and strong cytoplasmic positivity for CK20 (Panel D), along with nuclear positivity for CDX2 (Panel E) and SATB2 (Panel F). The tumor cells were negative for CK7. Mismatch repair protein staining demonstrated complete loss of MLH1 (Panel G) and PMS2 (Panel H), while MSH2 and MSH6 expression was preserved.
Signet-ring cell carcinoma (SRCC) is a rare and aggressive subtype of colorectal carcinoma, accounting for approximately 1% of cases and officially recognized by the WHO. It is defined histologically by the presence of signet-ring cells in more than 50% of the tumor, characterized by prominent intracytoplasmic mucin that displaces and molds the nucleus.
SRCC typically arises in the right (proximal) colon and often presents at an advanced stage, with a prognosis poorer than that of conventional adenocarcinoma or mucinous carcinoma. It exhibits a distinctive metastatic pattern, spreading rapidly and frequently to atypical sites such as lymph nodes, the peritoneal surface, and ovary, while liver involvement is less common.
Molecularly, SRCC is associated with a high incidence of microsatellite instability (MSI), a slightly lower rate of KRAS mutations, and has strong ties to Lynch syndrome, but is also a common type of cancer in patients with inflammatory bowel disease. These tumors may also exhibit the MSI/PD-L1 phenotype, offering potential therapeutic targets.
Immunohistochemistry plays a crucial role in the differential diagnosis, particularly in cases of metastatic signet-ring cell carcinomas from other primary sites such as the stomach, breast, or bladder. The typical immunoprofile of colorectal SRCC includes positivity for CK20, CDX2, SATB2, MUC2, and MUC5AC, with negativity for CK7. Additional markers such as estrogen receptor, Hep Par 1 and E-cadherin can assist in distinguishing SRCC of colorectal origin from those of gastric or breast origin; for instance, reduced E-cadherin expression is more typical in gastric or breast SRCCs. While these markers aid in diagnosis, their specificity remains limited, and results should always be interpreted alongside clinical and histological findings to improve diagnostic accuracy.
For further reading
- Chu PG, Weiss LM. Immunohistochemical Characterization of Signet-Ring Cell Carcinomas of the Stomach, Breast, and Colon. Am J Clin Pathol. 2004;121(6):884–892
- An Y, Zhou J, Lin G, et al. Clinicopathological and Molecular Characteristics of Colorectal Signet Ring Cell Carcinoma: A Review. Pathol Oncol Res. 2021;27:1609859
- Chen B, Liu B, Yuan Z, et al. Colorectal Signet Ring Cell Carcinoma Presenting as Ulcerating Rectosigmoid Stricture. ACG Case Rep J. 2023;10:e01130
- Gulinac M, Mileva N, Miteva D, Velikova T, Dikov D. Primary Signet-Ring-Cell Carcinoma in the Colorectum: A Case-Based Literature Review. Gastroenterol Insights. 2024;15(3):632–646
- Ono Y, Yilmaz O. Emerging and under-recognised patterns of colorectal carcinoma morphologies: a comprehensive review. J Clin Pathol. 2024 Jun 19;77(7):439-451.
Presented by
Dr. Julia Azevedo, Porto, Portugal, and Dr. Cord Langner, Graz, Austria.