-
Die Universität
- Herzlich willkommen
- Das sind wir
- Medien & PR
-
Studium
- Allgemein
- Studienangebot
- Campusleben
-
Forschung
- Profil
- Infrastruktur
- Kooperationen
- Services
-
Karriere
- Arbeitgeberin Med Uni Graz
- Potenziale
- Arbeitsumfeld
- Offene Stellen
-
Diagnostik
- Patient*innen
- Zuweiser*innen
-
Gesundheitsthemen
- Gesundheitsinfrastruktur
Case of the Month
February 2025
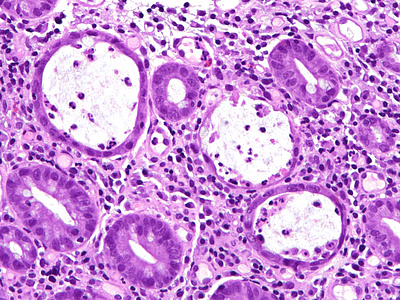
Colon biopsy from a 39-year-old female with history of malignant melanoma.
Diagnosis
Immune checkpoint inhibitor therapy-associated colitis.
Comment
A 39-year-old female was diagnosed with cutaneous melanoma pT3b with lymph node macrometastases five years ago. Over the past year, the patient had received 16 courses of Pembrolizumab. Subsequently, she was diagnosed with liver metastases of melanoma, and her immunotherapy regimen was changed to Ipilimumab plus Nivolumab. After the second course of Ipilimumab plus Nivolumab, the patient complained of worsening colic-like stomachache and diarrhea. Abdominal CT scan suggested pancolitis, and rectosigmoidoscopy revealed left-sided colitis.
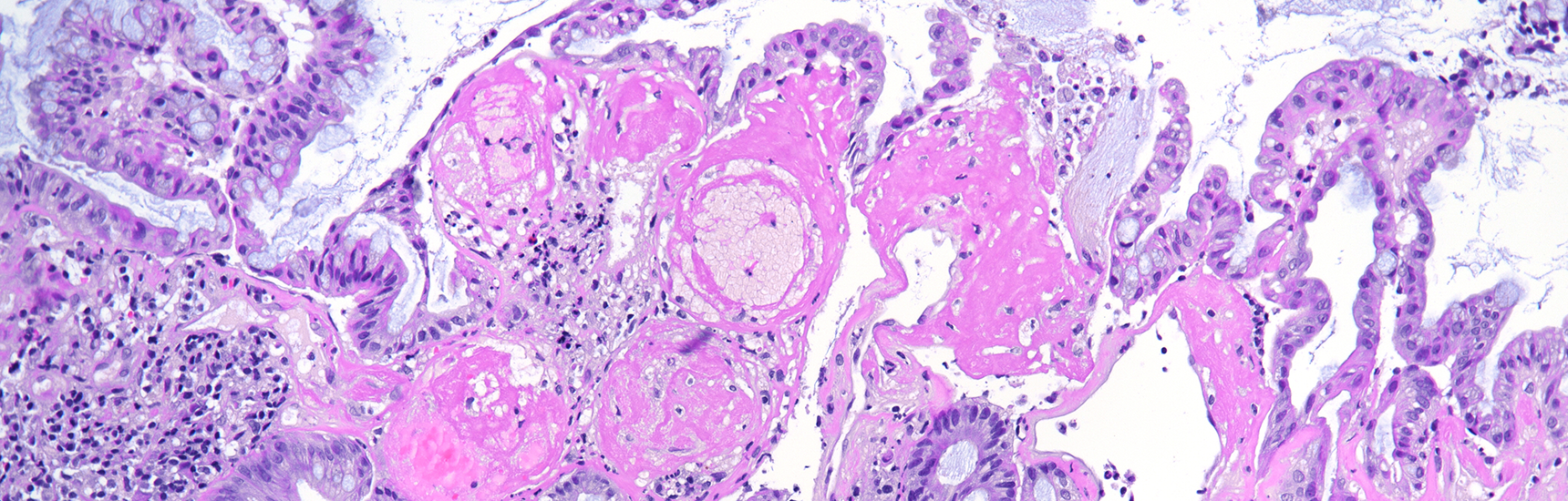
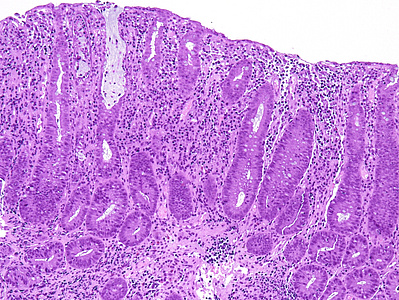
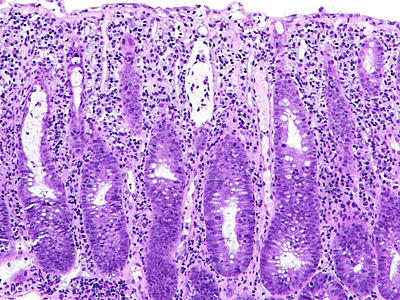
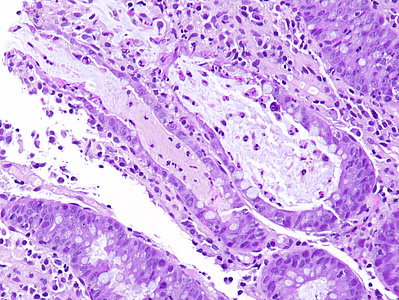
Histology showed mild crypt architecture distortion, increased lamina propria cellularity with mixed inflammatory cell infiltration containing plasma cells, lymphocytes, neutrophils, and scattered eosinophils. Mild basal plasmacytosis was present. The superficial epithelium was flattened and focally eroded (Panels A-B). Crypts showed a prominent loss of goblet cells, with reduced secretion from the remaining ones. Neutrophilic cryptitis with the presence of apoptotic bodies in the epithelial lining was observed. Some crypts were attenuated, lined by flattened epithelium, and contained apoptotic debris and neutrophils. Scattered withering crypts were found (Panels C-D).
These morphological findings of chronic active colitis with increased crypt epithelial apoptosis are suggestive of drug-induced colonic mucosa injury. Considering the patient’s known drug history of Pembrolizumab, Ipilimumab, and Nivolumab treatment, the diagnosis of immune checkpoint-inhibitor (ICI) therapy-associated colitis was made.
Immune checkpoint inhibitors (ICIs), increasingly used for the treatment of advanced cancers of various types, are known to cause mucosal injury in the gastrointestinal tract. The histologic features of ICI therapy-associated colitis include intraepithelial lymphocytosis, prominent apoptosis, and active inflammation. Histological patterns of colon injury observed in ICI therapy-associated colitis include active colitis, chronic active colitis, lymphocytic colitis, collagenous colitis, graft-versus-host-like colitis, and colitis with mixed patterns of injury. During the course of ICI therapy-associated colitis, in relapses or after switching to another drug type, the pattern of mucosal injury may change. ICI therapy-associated colitis may mimic inflammatory bowel disease (IBD) both clinically and morphologically, or, in some cases, “unmask” IBD. Therefore, a full clinical history, including drug history, is necessary for a pathologist to make a correct diagnosis.
For further reading
- Chen JH, Pezhouh MK, Lauwers GY, Masia R. Histopathologic Features of Colitis Due to Immunotherapy With Anti-PD-1 Antibodies. Am J Surg Pathol. 2017 May;41(5):643-654. doi: 10.1097/PAS.0000000000000829. PMID: 28296676.
- Tomm NK, Szczepanski JM, Fang JM, Choi WT, Xue Y, Setia N, Karamchandani DM, Cheng JY, Westerhoff M. Follow-up biopsies in gastrointestinal immune checkpoint inhibitor toxicity may show markedly different inflammatory patterns than initial injury. Hum Pathol. 2024 Jun;148:60-65. doi: 10.1016/j.humpath.2024.05.001. PMID: 38734079.
- Karamchandani DM, Westbrook L, Arnold CA. Drug-induced digestive tract injury: decoding some invisible offenders. Hum Pathol. 2023 Feb;132:135-148. doi: 10.1016/j.humpath.2022.06.014. Epub 2022 Jun 14. PMID: 35714837.
- Herlihy N, Feakins R. Gut inflammation induced by drugs: Can pathology help to differentiate from inflammatory bowel disease? United European Gastroenterol J. 2022 Jun;10(5):451-464. doi: 10.1002/ueg2.12242. Epub 2022 May 28. PMID: 35633273; PMCID: PMC9189468.
Presented by
Dr. Hanna Lapsar, Kyiv, Ukraine, and Dr. Cord Langner, Graz, Austria.