-
Die Universität
- Herzlich willkommen
- Das sind wir
- Medien & PR
-
Studium
- Allgemein
- Studienangebot
- Campusleben
-
Forschung
- Profil
- Infrastruktur
- Kooperationen
- Services
-
Karriere
- Arbeitgeberin Med Uni Graz
- Potenziale
- Arbeitsumfeld
- Offene Stellen
-
Diagnostik
- Patient*innen
- Zuweiser*innen
-
Gesundheitsthemen
- Gesundheitsinfrastruktur
Case of the Month
June 2025
Subtotal gastrectomy in an 84-year-old woman with a large antral ulcer.
Diagnosis
Gastric carcinoma with lymphoid stroma.
Comment
An 84-year-old female patient presented with deeply excavated ulcer involving the gastric antrum and extending into the pyloric region. Biopsies were performed, followed by subtotal gastrectomy. Gross pathological dissection of the resected specimen demonstrated a well-delineated, ulcerated lesion measuring 5cm in greatest diameter, located near the distal / duodenal resection margin.
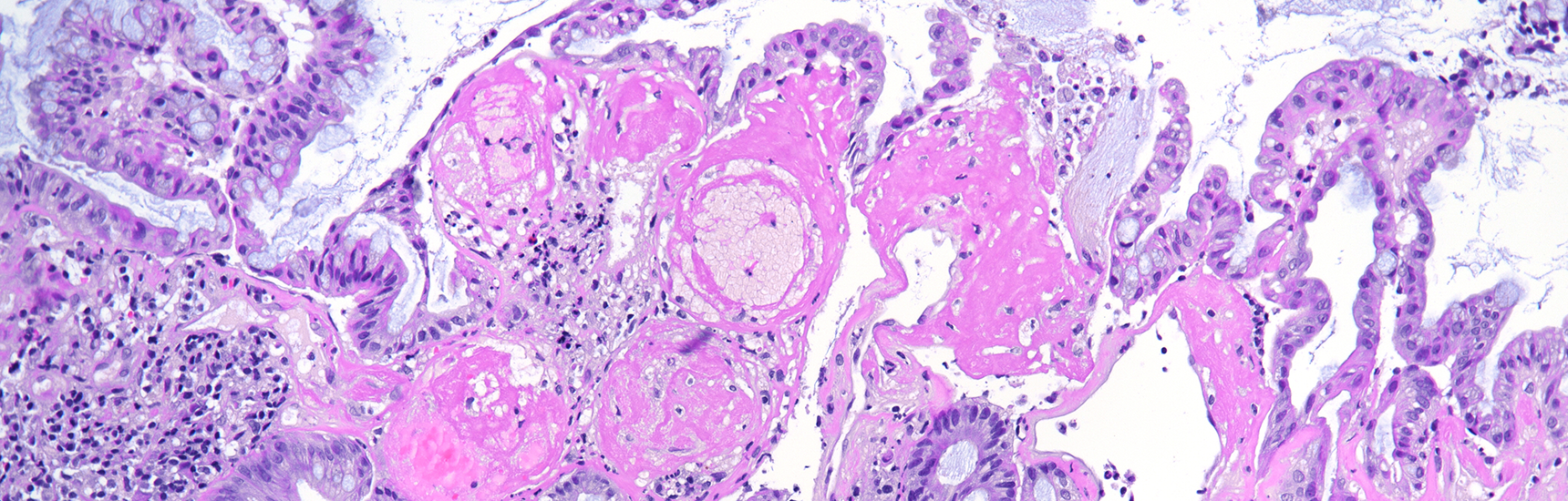
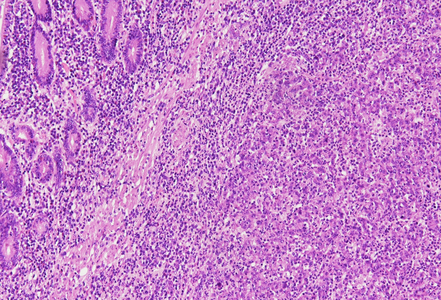
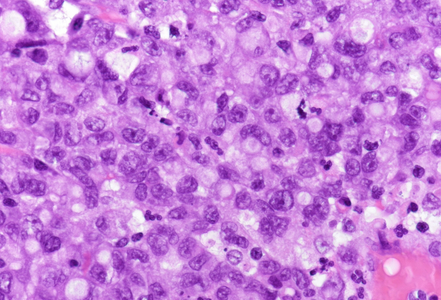
Histology showed a well-circumscribed carcinoma (Panel A) composed of irregular cords and single cells displaying a syncytial growth pattern (Panel B).
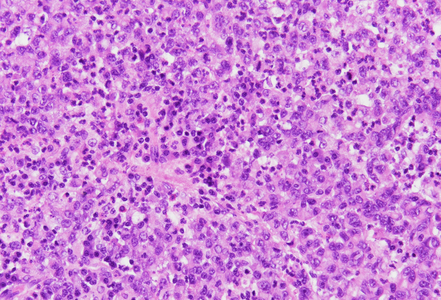
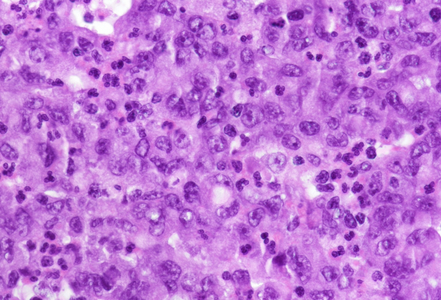
The neoplastic epithelial component was surrounded by a dense lymphoplasmacytic infiltrate, composed predominantly of small mature lymphocytes and neutrophils (Panel B and C). This inflammatory background obscured the malignant cells in some areas, contributing to the characteristic lymphoepithelioma-like morphology. The tumor cells were large, with vesicular, pleomorphic nuclei showing coarse chromatin, prominent nucleoli and abundant eosinophilic cytoplasm with indistinct cell borders (Panel D).
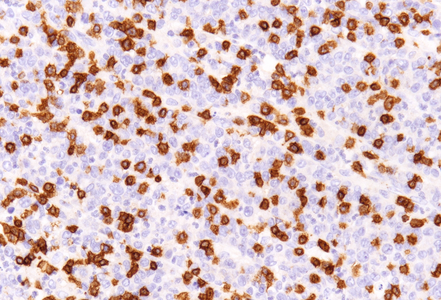
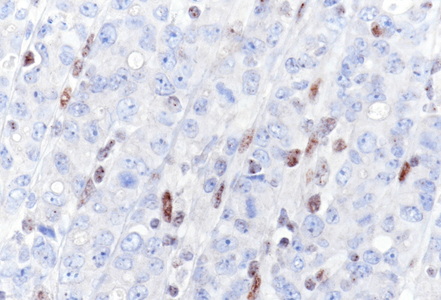
Immunohistochemistry for CD3 demonstrated lymphocytic infiltration within the tumor cell nests (Panel E). Staining for mismatch repair proteins revealed complete loss of MLH1 (Panel F) and PMS2 expression, while MSH2 and MSH6 were preserved. In situ hybridization for Epstein–Barr virus-encoded RNA (EBER-ISH) was negative.
Gastric carcinoma with lymphoid stroma, also known as lymphoepithelioma-like carcinoma or medullary carcinoma, represents a rare histological variant, accounting for approximately 1–7% of all gastric carcinomas. This entity is considered a poorly differentiated carcinoma composed of small trabeculae, solid nests, or sheets of epithelial cells embedded within a dense lymphoid stroma, closely resembling the morphological pattern seen in undifferentiated nasopharyngeal carcinoma.
Although the predominant inflammatory background is composed of mature lymphocytes and plasma cells, the presence of neutrophilic infiltration may also be observed, as demonstrated in the present case. This feature, even though not discussed in detail in larger case series, is diagnostically significant. Neutrophils can obscure the lymphocytic component and potentially be misleading, that is, distracting from accurate diagnosis, thereby constituting a potential diagnostic pitfall.
This type of carcinoma is strongly associated with Epstein-Barr virus (EBV) infection, with EBV positivity observed in over 80% of cases. Additionally, a small subset exhibits microsatellite instability (MSI) and/or mismatch repair deficiency. Important to note, EBV positivity and MSI are considered mutually exclusive events in gastric carcinoma pathogenesis.
These tumors frequently exhibit programmed death-ligand 1 (PD-L1) overexpression, rendering them susceptible to immune checkpoint blockade therapy. From a prognostic standpoint, this entity is associated with a more favorable outcome when compared to conventional gastric adenocarcinoma. Notably, MSI cases demonstrate a better outcome, independent of other factors such as tumor stage or nodal status.
For further reading
- Huh CW, Jung DH, Kim H, Kim H, Youn YH, Park H, Kim JW, Choi SH, Noh SH, Kim JH. Clinicopathologic features of gastric carcinoma with lymphoid stroma in early gastric cancer. J Surg Oncol. 2016 Nov;114(6):769–772
- Pyo JS, Kim NY, Son BK, Lee HY, Oh IH, Chung KH. Clinicopathological features and prognostic implication of gastric carcinoma with lymphoid stroma. Gastroenterol Res Pract. 2020;6628412:1-9
- Cui YJ, Ren YY, Zhang HZ. Treatment of gastric carcinoma with lymphoid stroma by immunotherapy: A case report. World J Clin Cases. 2022 Sep 6;10(25):8962–8967
- Gonzalez RS, Cates JMM, Revetta F, McMahon LA, Washington K. Gastric carcinomas with lymphoid stroma: categorization and comparison with solid-type colonic carcinomas. Am J Clin Pathol. 2017 Dec 1;148(6):517–527
Presented by
Dr. Julia Azevedo, Porto, Portugal, and Dr. Cord Langner, Graz, Austria.