-
Die Universität
- Herzlich willkommen
- Das sind wir
- Medien & PR
-
Studium
- Allgemein
- Studienangebot
- Campusleben
-
Forschung
- Profil
- Infrastruktur
- Kooperationen
- Services
-
Karriere
- Arbeitgeberin Med Uni Graz
- Potenziale
- Arbeitsumfeld
- Offene Stellen
-
Diagnostik
- Patient*innen
- Zuweiser*innen
-
Gesundheitsthemen
- Gesundheitsinfrastruktur
News
Our skin forms a barrier against pathogens and prevents excessive water loss, ensuring that the body does not dry out. The outermost layer, known as the stratum corneum, plays a crucial role in this process. It consists of dead cells and fats that make the skin water-repellent and stable.
In diseases such as ichthyosis – ancient Greek for “fish” – this barrier fails. The skin dries out, becomes scaly and severely keratinized. This genetic disease is not yet curable. Those affected are dependent on special care products for the rest of their lives. A rare form of ichthyosis is the particularly painful Chanarin-Dorfman syndrome. It can even be fatal in newborns. Franz Radner from the Institute of Molecular Biosciences at the University of Graz and his team have now elucidated the molecular causes of this disease.
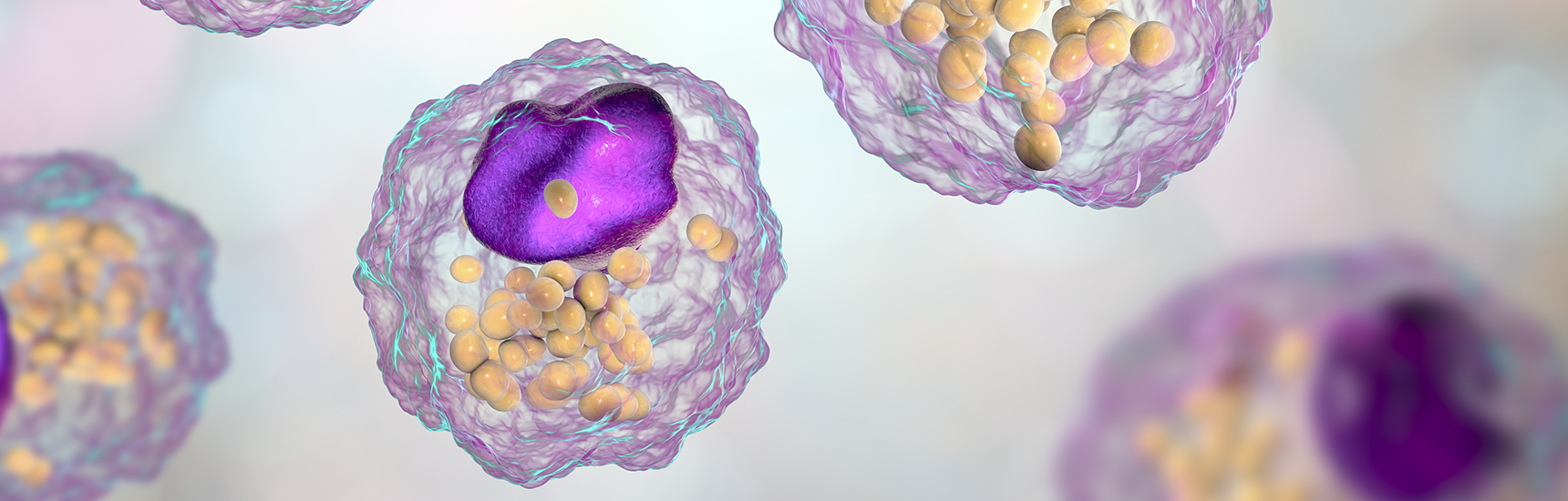
A lipid called acylceramide, which is essential for the formation of the skin barrier plays a key role. “Normally, the protein ABHD5 transports the enzyme PNPLA1 to the surface of small fat stores in the cell. There, PNPLA1 produces the vital acylceramide,” explains Radner. In a recent publication, the researchers describe their latest findings on this process: "Until now, we assumed that ABHD5 and PNPLA1 had to bind directly to each other for PNPLA1 to perform its enzymatic function. However, our study shows that spatial proximity is sufficient. But when mutations keep ABHD5 away from PNPLA1, acylceramide production collapses—and the skin barrier fails," says Radner, explaining the complex interaction of proteins, enzymes, and lipids in the body.
This knowledge opens up new therapeutic perspectives. Future approaches could aim to bring PNPLA1 to the right place in the cell even without ABHD5. In addition, initial findings show that skin creams containing acylceramide or similar lipids improve the skin barrier. Such strategies could not only help people with ichthyosis, but also alleviate age-related skin dryness.
Publication: Defective targeting of PNPLA1 to lipid droplets causes ichthyosis in ABHD5-syndromic epidermal differentiation disorder. Journal of Lipid Research. DOI: 10.1016/j.jlr.2025.100875.